
Chronic Pain Researchers have identified the precise location where a protein controls sodium ion channels, and they have successfully reduced pain in both cell and animal tests by introducing the genetic material of the channel into a virus.
In a recent study published in the Proceedings of the National Academy of Sciences (PNAS), researchers from NYU College of Dentistry’s Pain Research Centre created a gene therapy that cures chronic pain by indirectly controlling a particular sodium ion channel.
The specific location where a regulatory protein interacts to the NaV1.7 sodium ion channel to govern its activity has been identified, paving the way for the novel therapy that has been tested in both cells and animals.
“Our research constitutes a significant advancement in comprehending the fundamental biology of the NaV1.7 sodium ion channel, which can be utilised to alleviate persistent pain,” stated Rajesh Khanna, the NYU Pain Research Center’s director and a molecular pathobiology professor at NYU Dentistry.
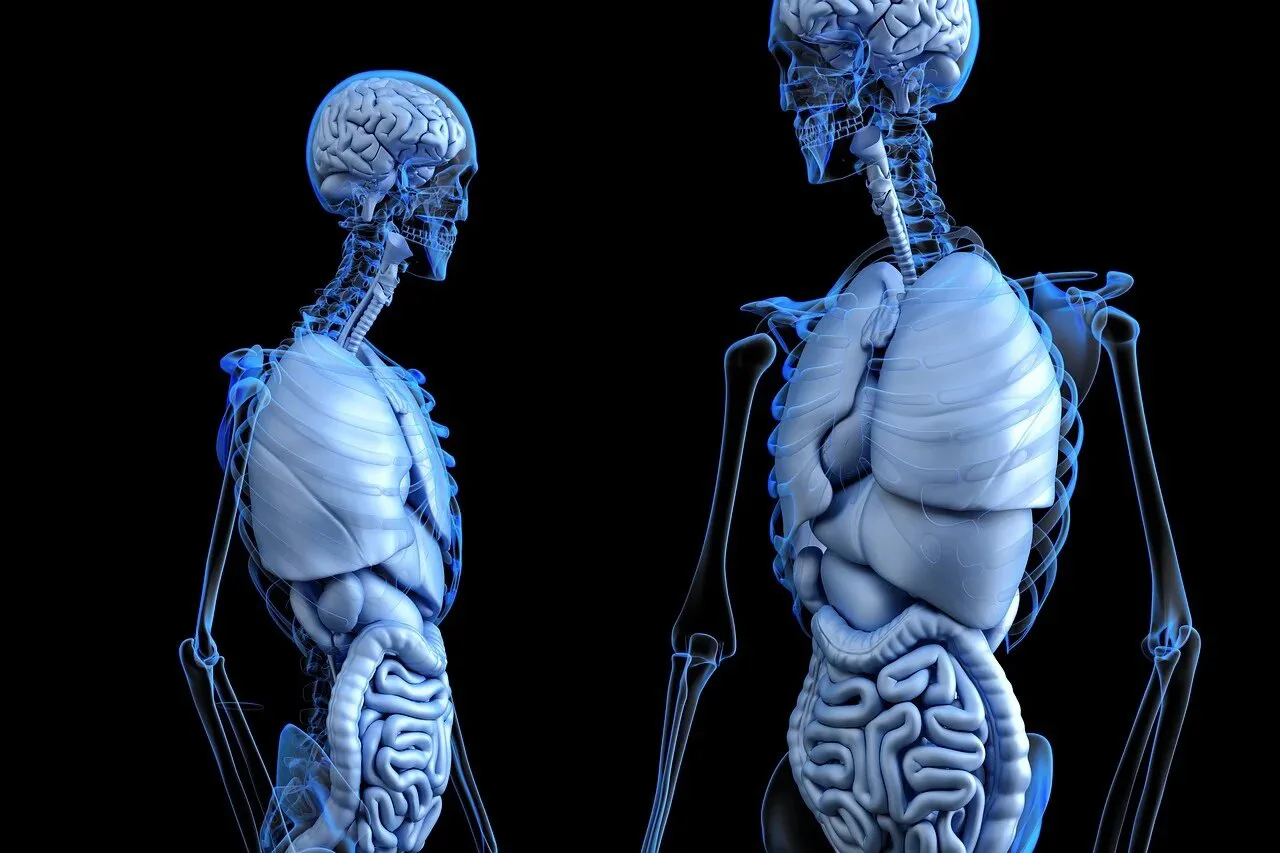
Roughly one-third of Americans suffer from chronic pain, which is a serious public health concern. Researchers are working hard to create safer and more effective painkillers than opioids.
Since sodium ion channels are essential for nerve cells, or neurons, to communicate with one another, they play a significant role in the development and transmission of pain. Once the significance of one specific sodium ion channel, NaV1.7, was identified in individuals with uncommon, genetic pain illnesses, it became a prospective target for pain treatment. A mutation in the NaV1.7 gene in certain families causes a significant amount of sodium to enter cells, which results in excruciating chronic pain. Mutations blocking NaV1.7 cause total analgesia in other families.
With little success, scientists have spent years trying to create painkillers that selectively block NaV1.7. Khanna has adopted a different strategy: instead of suppressing NaV1.7, he wants to use a protein called CRMP2 to indirectly regulate it.
By modulating the sodium ion channel’s activity, CRMP2 “talks” to the channel and adjusts how much sodium can enter it. We can reduce the amount of sodium that is consumed if you impede the interaction between Nav1.7 and CRMP2 and obstruct their communication. According to Khanna, the senior author of the PNAS article, “this quiets down the neuron and pain is mitigated.”
A little chemical that targets CRMP2 and indirectly controls Nav1.7 expression was previously created by Khanna’s team. Research on the compound’s potential application in people is still ongoing, but it has shown promise in managing pain in cells and animal models. The reason why CRMP2 exclusively interacts with the NaV1.7 sodium ion channel and not the other eight sodium ion channels in the same family persisted, despite the compound’s apparent success.
The PNAS study identified a particular area of NaV1.7 where the sodium ion channel’s activity is regulated by the binding of the CRMP2 protein to the channel. The fact that CRMP2 did not attach to other sodium ion channels easily led them to conclude that this area is unique to NaV1.7.
“This really excited us because we knew that the regulation by CRMP2 would be lost if we removed that specific segment of the NaV1.7 channel,” Khanna added.
The researchers synthesised a peptide from the channel that matches to the region where CRMP2 binds to NaV1.7 in order to restrict the communication between CRMP2 and NaV1.7. To deliver the peptide to neurons and inhibit NaV1.7, they put it into an adeno-associated virus. One of the most innovative methods in gene therapy is the employment of viruses to deliver genetic material to cells. This method has been successful in treating blood disorders, eye ailments, and other uncommon conditions.
Mice with peripheral neuropathy brought on by chemotherapy and pain, including sensitivity to touch, heat, or cold, were administered the modified virus.
The animals’ suffering was reversed within a week to ten days, according to the researchers.
“We’ve discovered a way to infect an altered virus with a minuscule amount of genetic material derived from a protein found in all humans,” Khanna continued. . This is only the latest illustration of how gene therapy is about to go into a new area: the management of chronic pain.
The researchers duplicated their findings by suppressing NaV1.7 function in rodents as well as cells from primates and humans. While further research is needed, this is an encouraging sign that their strategy will convert into a human treatment.
“There is a critical need for new pain treatments, particularly for cancer patients suffering from chemotherapy-induced neuropathy.” “Our long-term goal is to develop a gene therapy that patients could use to treat these painful conditions and improve their quality of life,” Khanna added.
“Uncovering and focusing on a distinct NaV1.7 domain responsible for persistent pain,” In addition to Kimberly Gomez, the following people also have this name: Bryan McKiver, Edward Choi, Dongzhi Ran, Lisa Boinon, Samantha Perez-Miller, Paz Duran, Santiago Loya, Cheng Tang, Aida Calderon-Rivera, Liberty François-Moutal, May Khanna, Cynthia L. Madura, M.
The authors of the study, in addition to Khanna, are Kimberly Gomez, Paz Duran, Santiago Loya, Cheng Tang, Aida Calderon-Riva, May Khanna, and Samantha Perez-Miller from NYU Dentistry; Harrison J. Stratton, Liberty François-Moutal, Cynthia L. University of Arizona’s Madura, Shizhen Luo, Dongzhi Ran, and Lisa Boinon; Virginia Commonwealth University’s Bryan McKiver, Edward Choi, and M. Imad Damaj; and St. Louis University’s Aubin Moutal.
With funding from the National Institute on Drug Abuse (DA042852) and the National Institute of Neurological Disorders and Stroke (NS098772, NS120663, and NS119263), the research is being conducted. Patents covering the technologies detailed in the article are held by Khanna and a number of co-authors. Khanna is also a co-founder of the biotech businesses ElutheriaTx Inc. and Regulonix LLC, which are focused on developing non-opioid medications for chronic pain.
- Also Like: Top 10 Benefits Of Strength Training
